Full Length Research Article
Detection of MexR and MexZ efflux pump genes and assessment of the synergistic effect of amikacin and gentamycin with some efflux pump inhibitors in antibiotic-resistant Pseudomonas aeruginosa
Sara Hameed Rajab1*, Mayada Abdullah Shehan2
Adv. life sci., vol. 12, no. 3, pp. 503-508, August 2025
*- Corresponding Author: Sara Hameed Rajab (Email: sara.hameed@uoa.edu.iq)
Authors' Affiliations
2. Department of Biology, College of Science, University of Anbar, Anbar – Iraq
[Date Received: 13/12/2024; Date Revised: 28/02/2025; Available Online: 31/10/2025]
Abstract![]()
Introduction
Methods
Results
Discussion
References
Abstract
Background: A bacterium called Pseudomonas aeruginosa causes infections with high mortality rates and has the ability to rapidly acquire resistance to a variety of antibiotics.
Methods: A total of 118 clinical specimens from both males and females of different age groups were gathered between early September 2022 and the end of December 2022 from several hospitals in Al-Anbar city, Iraq. The sample sources were wounds, burns, urinary tract infections (UTI), and sputum. P. aeruginosa was identified through its microscopical properties, confirmed using the VITEK 2 automated system, followed by molecular detection using the 16S rRNA gene. The Kirby-Bauer disk diffusion method was used based on CLSI guidelines (CLSI, 2022) for the aminoglycoside antibiotics class. DNA extraction from the twenty isolates was conducted using Presto™ Mini gDNA Bacteria Kit. After that, molecular analysis of MexR and MexZ was performed using the PCR technique.
Results: Within this, 65 isolates were determined as P. aeruginosa from 118 samples. The proportion of P. aeruginosa isolates from wound samples was 27/65 (41.5%), while in the burn wound, Urinary tract infection (UTI), and sputum were 20/65 (30.8%), 14/65(21.5%), and 4/65(6.2%), respectively. The findings of the test for antibiotic resistance were Amikacin (73.84%), Gentamycin (81.53%), Netilmicin (33.84%), and Tobramycin (66.15%). The molecular analysis of MexZ genes from the twenty isolates showed the highest prevalence, 20/20 (100%), and the MexR gene 14/20 (70%). The antagonism of aminoglycoside antibiotics by divalent cations was found, and it is noted that the presence of divalent cations increased the antibiotic Minimum Inhibitory Concentration (MIC) values.
Conclusion: It was found that MexR and MexZ genes are widespread in P. aeruginosa isolates, which indicated elevated mexXY-OprM and MexAB-OprM gene expression in P. aeruginosa. These elevated efflux pumps of P. aeruginosa may influence antibiotic ion fluxes at the bacterial cell membrane, contributing to the improved resistance to aminoglycosides. The aminoglycoside resistance isolates expressed decreased efflux pumps when inhibited by CCCP and Conessine.
Keywords: Pseudomonas aeruginosa, Efflux pump inhibitors, MexXY-OprM efflux system, Conessin
Pseudomonas aeruginosa is a bacterium from the family “Pseudomonadaceae”. Due to the risk to hospitalized patients, the mortality rate, antibiotic resistance, and production of extracellular toxins, this bacterium is among the most significant species [1]. Additionally, it contains significant virulence characteristics that compromise immune protection and result in substantial tissue damage [2]. This bacterium has intrinsic resistance to several types of antibiotics, leading to infections that are challenging to treat and that have a high morbidity and fatality rate [3]. Aminoglycosides are broad-spectrum antibiotics that gained prominence in the early 1940s with the discovery of streptomycin from a Streptomyces species [4]. Since then, at least ten aminoglycosides have been approved for clinical usage, with amikacin, gentamicin, netilmicin, and tobramycin being the most often used [5]. Reduced outer membrane permeability, active efflux pumps, and enzymes that alter aminoglycosides are the systems by which P. aeruginosa develop resistance to these antibiotics [6]. Efflux pump transport proteins play a role in extruding harmful substrates from inside cells to the external environment, thereby lowering intracellular antibiotic concentrations [7]. Antibiotic efflux resistance, which is accomplished by drug efflux pumps, is an important microbial resistance mechanism. Because the drug excretion rate is generally quicker than the drug penetration rate, the drug level in the cell may be regulated to a non-sensitive level [8]. P. aeruginosa has a higher prevalence of four of these efflux pumps: Resistance to aminoglycosides, beta-lactams, and fluoroquinolones can be caused by MexXY-OprM; resistance to fluoroquinolones can be caused by MexEF-OprN; and resistance to beta-lactams and fluoroquinolones can be caused by MexCD-OprJ and MexAB-OprM [9]. The MexXY operon, controlled by the MexZ, encodes MexXY components. MexXY is an inducible antibacterial. The induction of this system can be triggered by ribosome disruption [10]. MexAB-OprM expression is controlled by MexR, which inhibits the synthesis of MexAB-OprM [11]. A specific antibiotic causes bacteria with a mutant MexR gene to produce more MexA, MexB, and OprM proteins, which in turn causes efflux pumps to be overexpressed and antibiotic resistance to rise [12].
Efflux pump inhibitors (EPIs) are compounds that block efflux pumps through several methods [13]. Carbonylcyanide m-chlorophenylhydrazone (CCCP) is a well-known laboratory efflux pump inhibitor. It can be a potent inhibitor of RND EPs. It is a potent uncoupling agent that can stop the efflux pump from working by reducing the transmembrane electrochemical gradient and suppressing the chemical synthesis source, which in turn lowers the uptake of aminoglycosides by P. aeruginosa and lowers their bactericidal activity [14]. As well as conessine, it is a steroid alkaloid derived from the plant Holarrhena antidysenterica. It was isolated from a plant species in the Apocynaceae family. It possesses antimicrobial properties by inhibiting P. aeruginosa MexAB-OprM [15]. Indeed, in a number of P. aeruginosa cases of resistance to aminoglycosides in hospitals, the development of the resistant genes encoded by these antibiotics is a major problem. The current study was designed to study the resistance of P. aeruginosa to aminoglycosides, and also investigated the genetic basis of efflux pump-mediated aminoglycoside resistance in Pseudomonas aeruginosa isolated from clinical specimens through the detection of some antibiotic resistance-related genes, MexR, and MexZ in some isolated strains. Moreover, the study of the antibacterial activity of some aminoglycoside antibiotics and their synergistic interactions with efflux pump inhibitors, conessine, and carbonyl cyanide-m-chlorophenylhydrazone, against the isolated strains was also studied.
Sample collection and identification
A total of 118 clinical specimens from both males and females of different ages were gathered from the start of September 2022 to the end of December 2022, from patients at distinct province hospitals of Al-Anbar governorate, Iraq. The sample sources were wounds, burns, urinary tract infections (UTI), and sputum. The P. aeruginosa was identified through its cultural and microscopical properties [16] and confirmed by the pattern of biochemical profiles using the VITEK 2 automated system, followed by molecular detection using the 16S rRNA gene.
Antimicrobial Susceptibility Tests
The aminoglycoside antibiotics discs were selected: Amikacin, Gentamycin, Tobramycin, and Netilmicin. The diffusion method was applied to assess resistance for the bacterial isolates according to (CLSI-2022): A few colonies were added to brain-heart broth (2 mL) and cultured to obtain the bacterial suspension together with McFarland turbidity. A cotton swab was used to culture the bacterial suspension into Muller-Hinton agar plates. Antimicrobial discs were positioned on the medium's surface, then incubated at 37°C for 24 hours. The diameter of each antibiotic disk's inhibitory zone was measured and contrasted with the usual inhibition zone of CLSI-2022.
DNA isolation and molecular analysis
Following the guidelines provided by the manufacturer, genomic DNA was isolated from bacterial culture using DNA isolation kits (Geneaid, Korea). A Nanodrop device was used to measure the purity and concentration of the DNA, which was then stored at -20 °C to avoid deterioration. Molecular weight markers (100 bp), 1X (TAE) buffer, and 1% agarose gel were manufactured following the guidelines provided by the manufacturer. The sequences for the Mex R and Mex Z genes were verified by using the Nucleotide Blast program of NCBI. In the end, oligonucleotides of Reverse and forward primers synthesized by the BIONEER company (Korea), as described in Table 1, were selected
Preparation of PCR mixture
A PCR reaction of 25 μl was made of green master mix (Promega), template DNA, primer solution, and deionized water
Determination of minimum inhibitor concentration (MIC)
The Resazurin Microtitre Plate Assay (REMA) was used to assess the antibiotic solutions. 100 µl Mueller-Hinton broth was poured into each plate well under aseptic conditions. Next, 100 µl of the test substance was moved into the 96-well plates' first row. To do serial dilutions, 100 µl of the material was pipetted from the first row to the next rows in progressively decreasing concentrations as (1/2, 1/4, 1/8, 1/16, 1/32, 1/64, 1/128, and 1/256). Ten microliters of bacterial suspension (1.5 × 10⁸ CFU/mL) were added to each well [18].
Synergism between Carbonyl cyanide m-chlorophenylhydrazone and Conessine with aminoglycoside antibiotics: Checkerboard assay
To determine if two test materials combined in microtiter plates had an antibacterial impact, a checkerboard assay was employed. Each well of the initial microtiter plates received 100 μl of Mueller-Hinton broth (MHB) to maintain consistency with the MIC determinations. Next, 100 μL of the first test material was poured into the initial column, moving it vertically to the next wells and discarding the remaining 100 μL. To obtain a concentration in serial form 1/2 into 1/128, the second test substance (100 μL) was placed into the first row of a different microtitre plate, and another 100 μL was moved horizontally into the next wells, discarding the remaining 100 μL. Each concentration on the first microtitre plate receives a vertical transfer of the second material dilutions using a pipette. Each well received 10 µL of bacterial suspension (1.5×10⁸ CFU/mL). To prevent contamination, after being covered with Parafilm, the plates were incubated at 37°C for a full day. Following incubation, 100 μl of Resazurin was added to each well, and the plate was subsequently incubated again for 2–6 hours before results were read. The well that did not change color was then regarded as the intersection of the MICs of the two antibacterials used together. Following the calculation of each antibiotic's fractional inhibitory concentration (FIC), the Fractional Inhibitory Concentration Index (FICI) was computed. The FICI is most frequently used to define or characterize drug interactions.
The FIC for two antibacterials (B and A) working together is as follows:
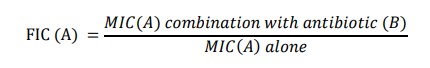
A: is the first test material, and B: is the second test material.
∑ FIC(FICI) is therefore given by:
FICI = FIC (A) + FIC (B)
A FICI value of ≤ 0.5 is indicative of a synergistic effect. FICI values > 0.5-4 are indicative of an additive effect (no drug interaction). Moreover, FICI > 4 indicates an antagonistic effect.
Synergy
A combination's MIC is at least two dilutions lower than the MIC of an antibiotic used alone, and its results are noticeably better than the sum of its independent activity when assessed separately.
Additive
When two medications are taken together, their effects are identical to those of the combination (the equally effective concentrations) when taken separately.
Antagonism
The combination's MIC is at least two dilutions higher than the MIC of the antimicrobial alone, and the combined result is noticeably worse than the best individual result [12].
Isolation of P. aeruginosa and identification
In this study, the collected samples were taken four months from the start of September until the end of December 2022. From 118 clinical specimens, 65 isolates were identified as P. aeruginosa, because of the microscopic examination that showed the P. aeruginosa colony, which has been colored pink, referred to as gram-negative, rod-shaped, non-spore-forming, single bacteria or arranged in pairs.
Antimicrobial Susceptibility Test
The disk diffusion method of Kirby-Bauer was applied to assess the antibiotic sensitivity of 65 P. aeruginosa samples. In accordance with (CLSI, 2022), susceptibility was tested toward the aminoglycoside antibiotics class, including amikacin, gentamycin, tobramycin, and netilmicin. The percentage of P. aeruginosa isolates shows high levels of resistance: 53/65 (81.53%) for Gentamycin, 48/65 (73.84%) for Amikacin, 43/65 (66.15%) for Tobramycin, and 22/65 (33.84%) for Netilmicin.
Molecular analysis
The molecular study for 20 isolates showed the percentage of the MexR gene was 14/20(70%), with a size product (637 bp) as shown in Figure 1. The results revealed that 20/20 (100%) isolates had the MexZ gene, as shown in Figure 2.
Determination of minimum inhibitor concentration by using Resazurin Microtitre-plate Assay (REMA) method
The results of MIC to the aminoglycoside group were: Amikacin (31.2 µg/mL) and Gentamycin (2.5 µg/mL) for both conessine and CCCP.
Evaluation of the effect of efflux pump inhibitors and an antibiotic solution combination using the checkerboard technique
The Checkerboard assay of P. aeruginosa gave synergistic profiles when efflux pump inhibitors (Conessine, CCCP) were combined with aminoglycoside antibiotics, separately (Table 2 & Figure 3). Minimum Inhibitory Concentration (MIC) of Amikacin alone for the test isolate was 31.2 µg/mL. When combined with the inhibitors, efficiency increased considerably. In the presence of conessine, the amikacin MIC decreased 4-fold from 31.2 to 7.81 µg/mL; with CCCP, it decreased 8-fold to 3.91 µg/mL. The inhibitors’ MICs in combination were 1.56 µg/mL (conessine) and 0.78 µg/mL (CCCP), respectively (Table 2). Since all FICI values were below 0.5, synergism is present, and as the number approaches zero, the degree of synergy increases.
Figures & Tables
In the findings of the current study, the highest percentage of P. aeruginosa in clinical isolates belongs to wounds, 27/65 (41.5%), followed by burns, 20/65 (30.8%). Kamali et al. [19] found that 10% of isolates that were obtained from the wound infection were P. aeruginosa. These results differed from our results. Another study, consisting of 235 different specimens in Baghdad city, revealed a percentage of clinical isolates (36%) of burns and (16%) of wound infection [20]. Due to their compromised immune system, prolonged hospitalization, and therapeutic and diagnostic procedures, burn patients are more likely than other patients to get infections. Furthermore, P. aeruginosa contamination of hospital air, equipment, and personnel's hands may be the origin of a significant portion of burn infections [21]. P. aeruginosa is a nosocomial infection that can occur during the implantation and removal of indwelling urinary catheters and contribute to urinary tract infections [22]. In critically sick pneumonia patients, admission to an intensive care unit (ICU) increases the possibility of P. aeruginosa infection [23]. A bacterium, P. aeruginosa, has shown resistance to the aminoglycoside group of antibiotics. Aminoglycoside resistance is mediated in P. aeruginosa via reduced outer membrane permeability, aminoglycoside modification enzymes, and an active efflux pump [6]. The percentage of the MexR gene found was 70% [24]. Also, the percentage of the MexR gene was found to be 79% [25]. Efflux pumps enable microorganisms to expel internal poisons, such as antibiotics. One of the largest MDR of efflux pumps, the MexAB-OprM pump is significantly expressed in P. aeruginosa and is regulated through the regulatory gene MexR. MexA, MexB, and OprM protein synthesis increase in response to antibiotic exposure in bacteria with the mutant MexR gene, which promotes the overexpression of efflux pumps and increases antibiotic resistance [23].
The results showed that the MexZ gene was detected in our study at a percentage of 100%, which indicates that the gene is widespread in isolates resistant to aminoglycosides. The MexZ repressor protein is often considered a key factor in the resistance of aminoglycosides in P. aeruginosa. Clinical isolates of P. aeruginosa frequently include MexZ mutations, which are linked to increased mexXY expression [26]. The most prevalent route by which P. aeruginosa imparts resistance to aminoglycosides is MexXY-OprM expression [27].
Patients who are bacteremic and have already been exposed to antibiotics may benefit from an antibiotic-inhibitor combo therapy [28,29]. Among all the tactics used to address the issue of resistance to antibiotics, surveillance of resistance to antibiotics is crucial. Alternative methods of dealing with infections caused by drug-resistant bacteria become necessary as a result of the rise in bacterial resistance to antibiotics and the dearth of newly available treatments [30]. Developing antibiotic substitutes and finding or creating adjuvants are two possible approaches that have been suggested [31]. Some attempts have been undertaken to boost or restore antimicrobial activity against germs that are resistant to multiple drugs [32]. When chemical inhibitors are added to antibiotics, the antibacterial MIC may decrease [33,34]. Finding ways to increase the antibiotics’ diffusion over bacterial membranes or to block the efflux pumps, which is a common resistance mechanism in Gram-negative bacteria, is essential in increasing the antibiotics’ effectiveness [35].
Acknowledgement
The authors acknowledge the College of Science, University of Anbar, Iraq, for providing research facilities.
Author Contributions
The authors shared the development, material preparation, and collection of the samples. Every author has read and approved the finished manuscript.
No conflicts of interest are disclosed by the authors.![]()
References
- Gani M, Rao S, Miller M, Scoular S. Pseudomonas mendocina bacteremia: A case study and review of literature. The American Journal of Case Reports, (2019); 20(2019): 453-458.
- Jawher IM, Hasan MG. Antibiotics resistance patterns of Pseudomonas aeruginosa isolated from meat at Mosul city retails. Iraqi Journal of Veterinary Sciences, (2023); 37(2): 363-367.
- Hossain MG, Saha S, Rahman MM, Singha JK, Mamun AA. Isolation, identification and antibiogram study of Pseudomonas aeruginosa from cattle in Bangladesh. Journal of Veterinary Advances, (2013); 3(7): 180–185.
- Khosravi AD, Mohammadian A. Efflux MexAB-mediated resistance in multidrug and pan-drug resistant strains of Pseudomonas aeruginosa isolated from patients with burn and wound infections. Jundishapur Journal of Natural Pharmaceutical Products, (2016); 11(1): e25352.
- Sahasranaman S, Howard D, Roy S. Clinical pharmacology and pharmacogenetics of thiopurines. European Journal of Clinical Pharmacology, (2008); 64(2008): 753–767.
- Seupt, A., Schniederjans, M., Tomasch, J., & Häussler, S. Expression of the MexXY aminoglycoside efflux pump and presence of an aminoglycoside-modifying enzyme in clinical Pseudomonas aeruginosa isolates are highly correlated. Antimicrobial Agents and Chemotherapy, (2020); 65(1): 1-11.
- Yaseen NN, Ahmed DA. Detection of mexB Multidrug Efflux Gene in Some Local Isolates of Pseudomonas aeruginosa. Iraqi Journal of Science, (2023); 64(1): 111-118.
- Poole K. Stress responses as determinants of antimicrobial resistance in Pseudomonas aeruginosa: multidrug efflux and more. Canadian Journal of Microbiology, (2014); 60(12): 783–791.
- Shigemura K, Osawa K, Kato A, Tokimatsu I, Arakawa S, et al. Association of overexpression of efflux pump genes with antibiotic resistance in Pseudomonas aeruginosa strains clinically isolated from urinary tract infection patients. The Journal of Antibiotics, (2015); 68(9): 568–572.
- Lorusso AB, Carrara JA, Barroso CD, Tuon FF, Faoro H. Role of Efflux Pumps on Antimicrobial Resistance in Pseudomonas aeruginosa, a Review. International journal of molecular sciences, (2022); 23(24): 15779.
- Jeannot K, Elsen S, Köhler T, Attree I, van Delden C, et al. Resistance and virulence of Pseudomonas aeruginosa clinical strains overproducing the MexCD-OprJ efflux pump. Antimicrobial Agents and Chemotherapy, (2008); 52(7): 2455–2462.
- Oumeri MM, Yassin NA. Molecular characterization of some carbapenem resistance genes among Pseudomonas aeruginosa isolated from wound and burn infections in duhok city, Iraq. Journal of Duhok University, (2021); 24(1): 136-144.
- Fodor A, Abate BA, Deák P, Fodor L, Gyenge E, et al. Multidrug resistance (MDR) and collateral sensitivity in bacteria, with special attention to genetic and evolutionary aspects and to the perspectives of antimicrobial peptides—a review. Pathogens, (2020); 9(7): 522.
- Naser HH, Aubaid AH. Molecular Detection and Quantification Gene Expression of Efflux Pump Antibiotic Resistance Genes in Extensive Drug Resistance Pseudomonas aeruginosa Isolated from Clinical Infection Patients in Al Diwaniyah City of Iraq. Medico-legal Update, (2020); 20(4): 41951.
- Rao M, Padyana S, Dipin KM, Kumar S, Nayak BB, et al. Antimicrobial compounds of plant origin as efflux pump inhibitors: new avenues for controlling multidrug resistant pathogens. Journal of Antimicrobial Agents, (2018); 4(1): 1-6.
- Gaby WL, Hadley C. Practical laboratory test for the identification of Pseudomonas aeruginosa. Journal of Bacteriology, (1957); 74(3): 356-358.
- Osman ME, El-Hendawy HH, Abd El-All SM, Hassan AM, Mahmoud DE. Correlation between resistance of Pseudomonas aeruginosa to benzalkonium chloride and expression of efflux pump genes. Journal of Applied Pharmaceutical Science, (2018); 8(12): 44–52.
- Elshikh M, Ahmed S, Funston S, Dunlop P, McGaw M, et al. Resazurin-based 96-well plate microdilution method for the determination of minimum inhibitory concentration of biosurfactants. Biotechnology Letters, (2016); 38(2016): 1015–1019.
- Kamali E, Jamali A, Ardebili A, Ezadi F, Mohebbi A. Evaluation of antimicrobial resistance, biofilm forming potential, and the presence of biofilm-related genes among clinical isolates of Pseudomonas aeruginosa. BMC Research Notes, (2020); 13(2020): 1–6.
- Al-Sheikhly MA, Musleh LN, Al-Mathkhury HJ. Gene Expression of pelA and pslA in Pseudomonas aeruginosa under Gentamicin Stress. Iraqi Journal of Science, (2020); 61(2): 295–305.
- Pachori P, Gothalwal R, Gandhi P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes & Diseases, (2019); 6(2): 109–119.
- Li Y, Ren L, Zou J. Risk factors and prevention strategies of nosocomial infection in geriatric patients. Canadian Journal of Infectious Diseases and Medical Microbiology, (2019); 2019(1): 1-5.
- Kello E, Greenberg R, Li W, Polansky S, Maldonado R, et al. The Effect of Antibiotic Treatment and Gene Expression of Mex B Efflux Transporters on the Resistance in Pseudomonas aeruginosa Biofilms. Applied Microbiology, (2023); 3(3): 709–721.
- Panahi T, Asadpour L, Ranji N. Distribution of aminoglycoside resistance genes in clinical isolates of Pseudomonas aeruginosa in north of Iran. Gene Reports, (2020); 21(2020): 100929.
- Llano-Sotelo B, Azucena EF, Kotra LP, Mobashery S, Chow CS. Aminoglycosides modified by resistance enzymes display diminished binding to the bacterial ribosomal aminoacyl-tRNA site. Chemistry & Biology, (2002); 9(4): 455–463.
- Prickett MH, Hauser AR, McColley SA, Cullina J, Potter E, et al. Aminoglycoside resistance of Pseudomonas aeruginosa in cystic fibrosis results from convergent evolution in the MexZ gene. Thorax, (2017); 72(1): 40–47.
- Hay T, Fraud S, Lau CH, Gilmour C, Poole K. Antibiotic inducibility of the mexXY multidrug efflux operon of Pseudomonas aeruginosa: involvement of the MexZ anti-repressor ArmZ. PLoS One, (2013); 8(2): e56858.
- Tang M, Wei X, Wan X, Ding Z, Ding Y, Liu J. The role and relationship with efflux pump of biofilm formation in Klebsiella pneumoniae. Microbial Pathogenesis, (2020); 147(2020): 104244.
- Osei Sekyere J, Amoako DG. Carbonyl cyanide m-chlorophenylhydrazine (CCCP) reverses resistance to colistin, but not to carbapenems and tigecycline in multidrug-resistant Enterobacteriaceae. Frontiers in Microbiology, (2017); 8(2017): 228.
- Siriyong T, Srimanote P, Chusri S, Yingyongnarongkul BE, Suaisom C, et al. Conessine as a novel inhibitor of multidrug efflux pump systems in Pseudomonas aeruginosa. BMC Complementary and Alternative Medicine, (2017); 17(2017): 1–7.
- Jewboonchu J, Saetang J, Saeloh D, Siriyong T, Rungrotmongkol T, et al. Atomistic insight and modeled elucidation of conessine towards Pseudomonas aeruginosa efflux pump. Journal of Biomolecular Structure and Dynamics, (2022); 40(4): 1480–1489.
- Kang CI, Kim SH, Park WB, Lee KD, Kim HB, et al. Clinical outcome of bacteremic spontaneous bacterial peritonitis due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae. The Korean Journal of Internal Medicine, (2004); 19(3): 160.
- Dey D, Debnath S, Hazra S, Ghosh S, Ray R, et al. Pomegranate pericarp extract enhances the antibacterial activity of ciprofloxacin against extended-spectrum β-lactamase (ESBL) and metallo-β-lactamase (MBL) producing Gram-negative bacilli. Food and Chemical Toxicology, (2012); 50(12): 4302–4309.
- Al-Wazni WS, Hadi BS. Antivirulence effects of pomegranate peel extracts on most common urinary tract infection pathogens in pregnant women. Journal of Contemporary Medical Sciences, (2015); 1(4): 7–12.
- Thakur V, Uniyal A, Tiwari V. A comprehensive review on pharmacology of efflux pumps and their inhibitors in antibiotic resistance. European Journal of Pharmacology, (2021); 903(2021): 174151.
This work is licensed under a Creative Commons Attribution-Non Commercial 4.0 International License. To read the copy of this license please visit: https://creativecommons.org/licenses/by-nc/4.0








