![]()
Infants-feeding practices and their relationship with socio-economic and health conditions in Lahore, Pakistan
Saadia Ijaz1*, Tayyaba Ijaz2, Raja Kamran Afzal3, Muhammad Masood Afzal1, Osama Mukhtar4, Nayab Ijaz2
Adv. life sci., vol. 2, no. 4, pp. 158-164, August 2015
*- Corresponding Author: Saadia Ijaz (Email: silverpinball@yahoo.com)
This article was processed offline.
Authors' Affiliations[Date Received: 16/06/2015; Date Revised: 20/08/2015; Date Published Online: 25/08/2015]
Abstract![]()
Introduction
Methods
Results
Discussion
References
Abstract
Background: Pakistan, has high infant mortality rate. Among every 1000 live births 0.76% becomes the victim of death due to malnutrition and fatal infections. Therefore, feeding modes and practices may serve as important factors for assessment of an infant's growth and nutritional status. This study was designed to assess the exclusive breast feeding rate, frequency of diseases during breast feeding, status of breast feeding along with weaning, level of education, occupation and socio-economic status of parents.
Methods: In the descriptive and cross-sectional study, a total of one hundred (100) infants were included. The sampling technique was non-probability convenience sampling. This study was conducted at vaccination centers and children clinics in different hospitals in city of Lahore -Pakistan.
Results: The results showed that 67% of the mothers exclusively breastfed their babies. 64% of the mothers had knowledge of exclusive breast feeding. The practice of breast feeding was found as 81% while artificial feeding was practiced among 19% of the mothers. Majority of the mothers started weaning their babies at the age 4 (31%) and 6 months (32%) whereas 28% mothers started after 6 months. 54% of mothers continued breastfeeding along with weaning. 72% of the mothers were aware of the importance of colostrum.
Conclusion: Maternal education and women's employment have been found major determinants for breastfeeding. The result indicates that in Pakistan, mothers receive counseling on breast feeding which is quite satisfactory and feeding practices of infants are found as better in Pakistan.
Keywords: Breast feeding, Weaning, Colostrum
Introduction
The period from birth to one year of age is the “critical window” for the promotion of good growth and development of a child. Therefore, to fulfill the evolving feeding requirements of infants, breast feeding should be initiated within one hour of birth. According to global recommendations for child nutrition breastfeeding must be continued exclusively for the first six months and after that they must receive nutritionally adequate safe, age appropriate and responsive complementary feeding [1].
Postnatal care offers an excellent opportunity to find out how the mother is getting along with her baby, particularly with regard to feeding. Infant feeding practices are inclined by socio-cultural and economic factors [2].
In Pakistan, the infant mortality rate is 76/1000 live births indicating that around 400,000 babies are likely to die during their first year of life [3]. The United Nations International Children’s Emergency Fund (UNICEF) has estimated that exclusive breastfeeding in the first six months of life can reduce under-five mortality rates in developing counties by 13% [3]. However, due to ignorance among general population and wrong marketing practices by the corporate sector, bottle feeding is becoming common among higher socioeconomic groups and working mothers [4, 5].
Breast milk has very high nutritious value. Breastfed infants have higher IQ and visual acuity, get fewer infections, and have better muscle development, and better respiratory function, proper digestive function and improved immunity [7]. Breastfeeding is considered an important indicator of assessment of baby’s growth and nutritional status [8, 9].
Weaning should be started when the baby is six months old. It is a gradual process which is carried out for sustainable growth beyond six months. So an infant’s diet should be supplemented with suitable foods rich in proteins and other nutrients. The weaning period is the most crucial period in development of a child, as during this period, children are particularly exposed to the deleterious synergistic interaction of malnutrition and infection [10]. Proper feeding practices will also help in achieving millennium development goals which calls for eradicating extreme poverty, hunger and reducing child mortality. Breastfeeding significantly contributes to low cost, high quality food and sustainable food security for a baby. By properly following the health feeding practices, child mortality can be reduced [11].
This particular study was focused on analyzing the practices of breastfeeding among infants, 9-12 months of age in different socioeconomic setups of our society starting from colostrum, exclusive breastfeeding, weaning supplementary foods and their overall impact on the infants. It also included the factors leading to avoid breastfeeding and those contributing to improper weaning of the child.
Objectives of this study are outlined here;
· To assess the prevailing feeding practices of babies in the community
· To determine the awareness about colostrum and its importance among the breastfeeding mothers
· To assess the exclusive breast feeding rate among the mothers.
· To investigate the reasons and causes of feeding other than breastfeeding. To correlate the impact of level of education of mothers/parents, occupation and socioeconomic status on feeding practices of babies
Methods
Study Design:
Descriptive cross-sectional study
Setting:
Vaccination centers and out patients department of pediatrics in different hospitals of Lahore (Services Hospital, Children Hospital, CMH Hospital and Mayo Hospital)
Study population:
Mothers having infants attending vaccination centres and out patients department of paediatrics in hospitals including Services Hospital, Children Hospital, CMH Hospital and Mayo Hospital Lahore.
Sample Size:
100
Sampling Technique:
Non-probability Convenience Sampling. One hundred mothers, having children of age group up to 12 months, attending vaccination centers and out patients department of paediatrics in hospitals including Services Hospital, Children Hospital, National Hospital and Mayo Hospital Lahore.
Ethical consideration
Mothers were explained the purpose and benefits of the study. These mothers were interviewed on a pre tested Questionnaire after taking an informed consent to participate in the study. Anyone having children of other age group or who refused to participate was excluded. The data was collected by on – job trained students.
Study Variables:
· Age of the infant
· Sex of the infant
· Mode of delivery
· Vaccination status of infant
· Mother’s education
· Mother’s occupation
· Monthly income/ income per capita
· Family Type
· Practice of infant feeding
· Knowledge about Exclusive Breastfeeding
· Frequency and type of illness in infant
· Alternate milk given
· Knowledge and practices regarding Colostrum
· Health status of the infant
· Weaning practice
Results
The research was carried out on children up to 1 year of age. The age distribution in study population of 100 children was as follows; 3% children less than 3 months of age, 17% less than 6 months, 36%less than 9 months and44% were 9-12 months old. The majority of babies 57% were male while 43% were female.
The mode of delivery of most, 64% babies was spontaneous vaginal delivery. Spontaneous vaginal deliveries with episiotomy were 9% and 27% were LSCS. 85% of the children were completely immunized till age, 10% were completely unimmunized and 5% were partially immunized.
Mothers of 28% children were illiterate, most of the mothers were under matric (34%), 21% were under graduate and 17% were graduate and above. Most of them (84%) were housewives and 16% were working women. 20% of the babies belonged to those families whose family income was less than PKR 5000, most of them belonged to income group PKR 5000-PKR 10,000 (38%), 18% belonged to PKR 11,000- PKR 20,000 and 24% belonged to above PKR 20,000 income group. Babies belonging to nuclear families were 66% while belonging to extended families were 34%.
81% mothers breastfed their babies and 19% did not, so most of the mothers breastfed their babies. Most (64%) had knowledge about exclusive breastfeeding while 36% did not know about it. 67% mothers exclusively breastfed their babies and 13% did not, remaining 20% did not breastfeed their babies at all. Only 7% mothers exclusively breastfed their babies for less than 4 months, 15% for 4 months, most (35%) exclusively breastfed their babies for 6 months, 10% for more than 6 months and 13% did not exclusively breastfeed their babies.
28% breastfed babies had less than 2 episodes of illness per month, most of them (52%) had 2 per month,13% had 4 per month, 2% had 2 per month and 1% did not have any illness. Most of the breastfed babies (40%) had gastric infection, 28% had respiratory, 21% had both gastric and respiratory infections and 11% did not have any of these infections. 4% mothers had social reasons for not breastfeeding, 10% had personal and 10% had medical reasons while 1% had other reasons for not breastfeeding. Remaining 75% gave breastfeed to their babies. 52% mothers gave cow’s milk as an alternate to breastfeed, 38% gave infant formula milk, and 6% pasteurized milk, while 4% did not give any alternate milk. So the majority of mothers gave cow’s milk to their babies as an alternate to breastfeed. Most of the alternate milk fed babies (41%) had gastric infection, 25% had respiratory, 19% had both gastric and respiratory infections and 11% did not have any of these infections.
73% mothers gave colostrum to their babies and 27% did not. The perception of 72% mothers about colostrum was that it is useful for the babies, 13% thought that it is unhealthy and 15% did not know about colostrum. Most of the babies (85%) had normal growth, 8% did not grow normally and 7% babies had average growth.
31% mothers started weaning at 4th month of age, 32% at 6th months, 28% after 6 months and 9% had not yet started. Most of the babies had normal growth during weaning and 9% had not. Remaining 9% had not yet started weaning. 54% mothers continued breastfeeding along with weaning and 46% did not.
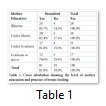
The percentage of those mothers who did not breastfeed their babies increased with increase in education of the mothers. 85.7% illiterate mothers breastfed their babies and this percentage decreased to 82.4%, 81% and 70% in under matric, under graduate and graduate or above respectively (table 1).
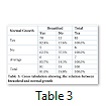
92.1% mothers who breastfed their babies, had monthly income of PKR 5000- PKR 10,000 while mothers having monthly income above PKR 20,000 had least breastfeeding percentage 78.8% (table 2). Among the babies who did not have normal growth, 37.5% were not being breastfed by their mothers while 17% and 14% non-breastfed babies had normal and average growth respectively (table 3).
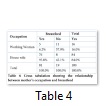
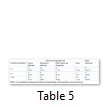
Among mothers who did not breastfed their babies 57.9% were working women. Out of 16 working women 11 did not breastfeed their babies (table 4). Among the babies who were not exclusively breastfed, 39% had gastric infection, 30% had respiratory, 18% had both gastric and respiratory infections and 13% did not have any of these infections. While those babies who were not exclusively breastfed did not show any difference in disease (table 5).
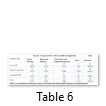
Out of alternate milk fed babies, those feeding on cow s milk had greatest frequency of infections having 46.2% gastric, 21.2% respiratory, 23% both gastric and respiratory infections. Babies feeding on infant formula milk mostly had gastric infections (39.5%), the percentage of those having respiratory and both gastric and respiratory infections were 26% and 18% respectively. Pasteurized milk feeding babies mostly had respiratory infections (67%), while the percentage of gastric infections and both gastric and respiratory infections were 33% and 0% respectively (table 6).
Data and Figures
Discussion
Subject study was conducted to explore and describe feeding practice of infants visiting at vaccination centers and outpatients department of paediatric in hospitals including Services, Children, National and Mayo hospital. 100 mothers were interviewed from different socioeconomic background. All of them had babies ranging from 3 months to 12 months of age groups.
The main purpose of this study was to assess the exclusive breastfeeding rate. Our study showed that 67% mothers exclusively breastfed their babies and 13% did not. Among exclusively breastfed babies, 35% were exclusively breastfed for 6 months which is lower than the exclusive breastfeeding rate in another study conducted in Karachi [12]. In our study a decline in exclusive breastfeeding after 4 months was observed (32%). This decline in exclusive breastfeeding after 4 months is seen in most developed countries of the world. Factors affecting breastfeeding have been reviewed extensively [13-15]. Maternal education and women's employment were two major determinants described by most of these reviews. In this study, the percentage of mothers who didn't breastfed their babies increased with the increase in education. 85.7% illiterate mothers breastfed their babies and this decreased to 82.9%, 81% and 70% in under matric, under graduate and graduate or above respectively. Singh et al [15] reported that only 4.6% illiterate mothers were breastfeeding. Similar trends were observed in the working mothers. Among working mothers only 6.2% were breastfeeding i.e. 11/16 were not breastfeeding. So mothers’ employment was found to have a significant negative influence on the breastfeeding practices. So, it is concluded that there is strong association between mothers’ occupation and breastfeeding.
Our study showed that most of the mothers (92.1%) which breastfeed their babies have monthly income of 5,000-10,000 while mothers which have monthly income of 20,000 and above have least breastfeeding percentage (70.8%). There was observed an increasing trend towards the use of artificial feeds among high income subjects. The reason may be that the mothers having high monthly income can afford artificial feeds as compared to the mothers having low income.
As far as the gastric & respiratory infections are concerned, our study showed no relationship between these infections and breast fed babies or bottle fed babies. However another study showed that the rate of infections increased among the babies who were using artificial feeds [16].
As far awareness of colostrum and its importance is concerned, majority of the participants (72%) of this study thought it as useful for the babies. Only 13% thought it as unhealthy. Remaining 15% didn't know about colostrum. Almost two-third of the mothers were aware of the importance of colostrum. But the percentage of negative perception and no knowledge of colostrum was also noticeable.
In spite of widespread practices of breastfeeding (81%) which is quite higher than the breastfeeding rates in the other studies artificial feeding was practiced among 19% of the mothers [17,18]. This small percentage of mothers practicing artificial feeding is due to the fact that in Pakistan, mothers receive counseling on appropriate breastfeeding. So this is quite satisfactory. The reason among mothers who didn’t breastfeed their babies were maternal serious illness, insufficient milk and occupational problems. Almost same reasons were quoted in the study of Kuwait, India and mini survey study of Pakistan [14, 15, 18].
In our study, the most common artificial feeds used were cow's milk (52%), infant formula (20%), dried milk (18%) and pasteurized milk (6%). So cow’s milk was the most preferred artificial feed. Similar results were found in another research [19]. The prominence of cow's milk feeding in our study may be because of the reason that it is easily available and much cheaper than the products available in the market. The mothers using infant formula were mostly those who were suffering from illness and this artificial feed was prescribed by their physicians.
As far as weaning is concerned, majority of the mothers started weaning their babies at the age of 4 months (31%) and 6 months (32%). Whereas 28% mothers started after 6 months. 54% mothers continued breastfeeding along with weaning and 45% didn’t.
There were several limitations in our study. It was conducted among mothers who visited the hospitals and vaccination centers. They mothers were more likely to receive better health application, support and motivation to continue breastfeeding practice. Therefore clinic based sampling procedures may systematically overestimate the final proportion.
It is concluded after the study that most of the mothers (81%) breastfeed their babies whether the mothers are illiterate or educated but the frequency of breastfeeding is less in educated mothers. 67% mothers exclusively breastfed their babies. Most of the mothers (72%) have knowledge about the benefits of breastfeeding. Most of the mothers (63%) start weaning of their babies at the age of 6 and 4 months and (52%) mothers use cow milk as an alternative. 54% mothers continued breastfeeding along with weaning. Babies who were not breastfed suffered from infections more frequently. Socio-economic status, type and size of family did not has any effect on feeding practices.
References
- Batal M, Boulghourjian C, Abdallah A, Afifi R. Breast-feeding and feeding practices of infants in a developing country: a national survey in Lebanon. Public Health Nutrition, (2006); 9(03): 313-319.
- Setegn T, Gerbaba M, Belachew T. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: A cross sectional study. BMC Public Health, (2011); 11(1): 217.
- Turab A, Soofi SB, Ahmed I, Bhatti Z, Zaidi AK, et al. Demographic, socioeconomic, and health characteristics of the MAL-ED network study site in rural Pakistan. Clinical Infectious Diseases, (2014); 59(suppl 4): S304-S309.
- Zurayk H. A two stage analysis of the determinants of fertility in rural South Lebanon. Population Studies, (1979); 489-504.
- Brady JP. Marketing breast milk substitutes: problems and perils throughout the world. Archives of Disease in Childhood, (2012); 97(6): 529-532.
- Brodribb WE. Ethics and the WHO “International Code of Marketing of Breast-milk Substitutes”. Breastfeeding Medicine, (2014); 9(3): 170-170.
- Campoy C, Escolano-Margarit M, Anjos T, Szajewska H, Uauy R. Omega 3 fatty acids on child growth, visual acuity and neurodevelopment. British Journal of Nutrition, (2012); 107(S2): S85-S106.
- Gress-Smith JL, Luecken LJ, Lemery-Chalfant K, Howe R. Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Maternal and Child Health Journal, (2012); 16(4): 887-893.
- Popkin BM. Contemporary nutritional transition: determinants of diet and its impact on body composition. Proceedings of the Nutrition Society, (2011); 70(01): 82-91.
- Howie G, Sloboda D, Vickers M. Maternal undernutrition during critical windows of development results in differential and sex-specific effects on postnatal adiposity and related metabolic profiles in adult rat offspring. British Journal of Nutrition, (2012); 108 (02): 298-307
- Nordin SM, Boyle M, Kemmer TM. Position of the Academy of Nutrition and Dietetics: Nutrition security in developing nations: Sustainable food, water, and health. Journal of the Academy of Nutrition and Dietetics, (2013); 113(4): 581-595.
- Parveen N, Majeed R, Khawaja MA. Evaluation of breast feeding practices. Gomal Journal of Medical Sciences, (2004); 7(1).
- Li R, Fein SB, Chen J, Grummer-Strawn LM. Why mothers stop breastfeeding: mothers' self-reported reasons for stopping during the first year. Pediatrics, (2008); 122(Supplement 2): S69-S76.
- Morisky DE, Kar SB, Chaudhry AS, Chen KR, Shaheen M, et al. Breastfeeding practices in Pakistan. Pakistan Journal of Nutrition, (2002); 1(3): 137-142.
- Singh P, Bhalwar R. Breast feeding practices among families of armed forces personnel in a large cantonment. Medical Journal Armed Forces India, (2007); 63(2): 134-136.
- Softić I, Atić N, Tahirović H. Infant feeding in respiratory and gastrointestinal infections during the first six months of life. Medicinski Arhiv, (2007); 62(1): 14-17.
- Javed N, Zaidi N, Khan MA. To Assess the Relations Between Breast Feeding and Illness in Children under Two Years of Age with Particular Reference to Respiratory Tract Infections. Pakistan Journal of Medical Research, (2008); 47(4): 92-94.
- Al Awadi FA, Amine EK. Recent trends in infant feeding patterns and weaning practices in Kuwait. Eastern Mediterranean Health Journal, (1997); 3(3): 501-510.