Review Article
Awareness of Asthma Genetics in Pakistan: A Review with Some Recommendations
Muhammad Farooq Sabar1*, Muhammad Akram1, Farheena Iqbal Awan1, Muhammad Usman Ghani1, Mariam Shahid2, Zafar Iqbal3, Samra Kousar2, Muhammad Idrees1
Adv. life sci., vol. 6, no. 1, pp. 1-10, November 2018
*- Corresponding Author: Muhammad Farooq Sabar (Email: farooqsabar@yahoo.com)
Authors' Affiliations
2- CEMB, University of the Punjab, Lahore, Pakistan
3- King Saud Bin Abdulaziz University for Health Sciences, KSA, Saudi Arabia
Abstract![]()
Introduction
Methods
Discussion
Conclusion
References
Abstract
About 334 million people worldwide have been affected by asthma and additionally 100 million expected to have asthma by the year 2025. Being the sixth most populous and economically developing country and with the increasing trend of urbanization and due to poor health facilities, lacking the knowledge of the causes of the disease, increased pollutant exposures and consanguineous marriages, Pakistani population has greater chances of asthma and allergic diseases. Almost 20% of overall pediatric population of Pakistan is affected by this disease. In the past, only environmental factors were considered responsible for asthma but now it is a well-known fact that genetic factors have major contribution in the development of the disease. Poor knowledge of the possibility of genetics involved in this disease has been very common in both uneducated as well as educated population of this region. There is no doubt today that genetics have a major role in the exhibition of asthma but unlike other Mendelian disorders it cannot easily be identified by a single or a simple set of associated genes, rather small contributions of multiple genes and environmental exposure to asthmatic patients may be found. Our focus in this article is genetic factors of asthma in Pakistan. More than 100 genes associated with asthma have already been reported in different populations worldwide but generally, due to an ignored disease in this region, possible genetic causes, impacts, management and treatment of the disease has rarely been studied in Pakistan. This article was intended to explore some latest developments in asthma genetics, diagnosis, prognosis and management and suggest some recommendations to control this deadly disease.
Keywords: Asthma genetics, Asthma prevalence in Pakistan, Genetic variants and asthma, Asthma genetic factors, Asthma genetic studies
Asthma is a chronic bronchial and inflammatory disorder of airways. It is exploited by multiple cellular elements and immune cells which include T-lymphocytes, mast cells, macrophages, neutrophils, epithelial cells and eosinophils. In asthmatic patients, the immune response leads to coughing, recurrent wheezing episodes, chest tightness and breathlessness [1]. A high pitch whistling and variable airflow obstruction are the visible symptoms of asthma susceptibility [2].
Globally asthma is one of major chronic disease [3] and its prevalence is continuously increasing [4] especially in low and middle income countries [5]. The statistical data of few decades have shown increased prevalence in both children and adults which may be due to changes in indoor-outdoor environment, climate and lifestyles [3,6]. Due to increased prevalence of asthma and higher morbidity rate, asthma has become a major global health concern [4].
Multiple risk factors, including poor compliance, non-affordability of medications, lack of follow-ups, incorrect perception of the use of inhalers, non-availability of healthcare facilities, lower socioeconomic status, lack of proper education, along with environmental triggers and genetic aspects may be involved in the overall increase in the prevalence of the disease in different populations [7-9]. Being the sixth most populous and economically developing country and with the increasing trend of urbanization and western lifestyle population, Pakistan has the greater chances of asthma and allergic diseases due to an increased exposure of pollutants along with a trend of consanguineous marriages [10-12]. We searched literature regarding the status of prevalence, diagnosis, management, mortality and understanding of genetics or genes involved in asthma. A special focus was Pakistan and other neighboring countries. We have found that it is mostly the ignored disease in the countries like Pakistan and rarely has been studied. Genetic variants and factors involved in the disease development had rarely been investigated in Pakistan in the past until few studies in the last five years [13]. This review is intended to discuss the level of understandings of genetics and status of diagnosis, prognosis, management and treatment of asthma in the region.
Literature survey and selection criteria
A systematic search was carried out from PubMed (NLM), Web of Science, Google Scholar and Google Web Browser by providing key terms “asthma, asthma Genetics, asthma prevalence, asthma risk factors, asthma management, asthma pharmacogenomics etc”. The literature found was further screened for inclusion according to their contents. In this study, more than 100 peer reviewed research articles were selected.
ASTHMA PREVALENCE AND PAKISTAN
Currently, approximately 334 million people around the globe have been affected by asthma [3] and additionally 100 million expected by the year 2025 [4]. Yearly approximate worldwide death rate due to asthma is reported 180,000 [14]. Poverty, severe asthma and poor disease management are the main reasons for increase in asthmatic admission in hospitals [15,16]. There is higher rate of asthma in developed countries than developing countries, but now it is also increasing in developing countries due to urbanization [14].
In Pakistan, there is great variation in reported asthma prevalence ranging from 4.3% to 31.58% [4,17] in different areas. Indoor and outdoor air pollution in the region is representing a major cause of asthma [4]. Changes in life style and increasing urbanization, has significantly increased the asthma prevalence in Pakistan during the last decades and the number of asthmatics is expected to rise during the next decade [4]. In Central Asia and Pakistan, adequate therapy is often not received by many asthmatics due to many factors such as hesitation to use inhaler devices.
Karachi is the largest city of Pakistan and about 40% population of the city is living in high asthma risk environment [18]. 8-10% of its population is victim of chronic asthma. Almost 20% of overall pediatric population of Pakistan is affected with this disease [4]. Situation is alarming as according to an asthma report, prevalence is 31.58% in school going children of Islamabad [17], significantly higher than asthma prevalence in Karachi i.e., 15.8% [19]. In other countries, we see that it is 19.8% in Qatar [20], 12.5% in Tonga [21], 13.6% in Fiji [21], 20.3% in Cape Town [22], 20.9% in UK [23], 11% in Hong Kong [24] and 15% in India [25]. Globally, in children asthma prevalence has a large variation ranges from 1.6% to 28.2% in age group of 13-14 years and from 4.1% to 32.1% in age group of 6-7 years [26].
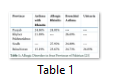
A local study on retrospective analysis of already diagnosed allergic patients was conducted at Allergy Center NIH, Islamabad during the year 2007. The study was designed to investigate the most prevalent allergic disorder in patients who visited the Allergy Center, National Institute of Health (NIH) Islamabad. Overall prevalence in Pakistan, according to this study, is 24.6 % for allergic rhinitis,24.04% for urticarial, 19.4% for bronchial asthma and 8.4% for eczema in age group of 12-55 years. Majority of the asthmatics of this population were reported as affected with environmental allergies [25]. Table 1 shows the percentage of allergic disorders in Pakistani population. Asthma diagnosis is extremely poor in Pakistan due to blemishes associated with asthma, lack of awareness and threat of life-long treatment. So, mass public awareness is needed to overcome these factors for early detection and treatment of asthma in Pakistan [27].
ASTHMA RISK FACTORS
Asthma risk factors can be divided in two main categories i.e., environmental and host factors. Environmental factors are not in the scope of this review so these will be discussed elsewhere and host factors only are discussed here.
Host Factors
These factors cause asthma development directly and include genetics, diet, obesity and gender [23]. The important host factors involving genetics are reviewed here.
Genetic factors: Asthma is a multi-factorial and polygenic complex disorder of airways which is believed to be by the genetic or environmental or the complex interaction of both genetic and environmental factors [28]. Asthmatic effects caused by the environmental exposure may be modulated by genomic sequence or mutated genomic regions but conversely environmental factors may also modulate the genomic expression by histone modification without altering genomic sequence and thereby altering asthma phenotype [29]. Asthma does not follow Mendelian Inheritance pattern but there is no doubt that genetics have a major role in the manifestation of asthma and multiple genetic factors contribute to the overall variations in the trait [30]. So, genetic association data could better help in diagnosis, understanding and management of asthma [31]. Being studied rarely in countries like Pakistan, especially its genetic factors, there is very little knowledge of its genetic implications in these countries.
Gender: Some studies from different parts of the world also showed that the risk factor for childhood asthma in males is higher than females as asthma prevalence is much higher in boys as compared to girls up to the age of 14 years [32-37]. But contrary to this, during adulthood, asthma prevalence is higher in women than [38-40]. The reasons are still unknown for this gender related difference in asthma prevalence during different ages. However lung size is larger in females as compared to males at birth but smaller in adulthood [23] which might be one reason. Sex related asthma prevalence studies in Pakistan resulted in the similar patterns [17,27,41].
Asthma onset: Asthmatic complication may start at any age and most of the children having asthma recovered before the age of 16 [3]. Asthma of adult age differs from childhood asthma which is more severe, often non-atopic and associated with higher decline in lungs function [42]. Asthmatic complications are expressed in majority of patients in early childhood [4]. As discussed earlier, asthma and wheeze prevalence is higher in males of early age while in elder age asthma is relatively more prevalent in females [43,44].
In spite of sharing some common genetic origins, several studies point out different genetic factors which differ in childhood asthma to adult-onset asthma [42,45]. 100kb region of 17q12–21 locus which includes ORMDL3, GSDMB, ZPBP2, IKZF3 genes is associated with childhood asthma susceptibility and extensively replicated in different studies [46-50]. This region is also associated with asthma in Pakistani population as reported in our recent publication [9]. DENND1B [51,52], ATPAF1 [53], PCDH1 [54], V4 variant of ADAM33 [55], IL-17A and IL-17 [56] and several other genetic loci have also predicted the genetic association with childhood asthma but 17q12–21 locus is most prominently replicated in number of studies [45].
In a GWAS studies on Japanese population, Tomomitsu and colleagues identified five adult asthma associated genetic loci which include two already reported loci “major histocompatibility complex (PMID: 10377184) and TSLP (PMID: 21804549) -WDR3 (PMID: 19198610)”. In this study they also identified USP38-GAB1 locus on chromosome 4q31, a locus on chromosome 10p14 and a gene-rich region on chromosome 12q13 as the new genetic loci associated with asthma susceptibility in Japanese adults [57]. The same group identifies another novel HAS2 gene in GWAS which was significantly associated with adult Japanese asthmatics having low smoking exposure [58]. The genetic variants of IL-13 [59,60], IL-4, IL-4R [61], HLA-G [62], GSTA1, GSTO2 [63], CC16 A38G [64], ORMDL3 [9], ADAM33 [13] and CCL5 [65] have also shown association with adult-onset asthma in different populations.
Other Allergic diseases: Clinical relationship of asthma with atopic dermatitis and allergic rhinitis is commonly called “allergic triad” [66]. Several studies suggest that food allergy and atopic dermatitis which develops during infancy leads to asthma or/and allergic rhinitis of childhood [67-70]. Asthma with allergic complications is a common childhood disease and experimental observations are strongly in favor of its genetic origin [71]. Approximately 30% children having atopic dermatitis build up asthma and about 66% develop the allergic symptoms and allergic sensitization [72]. The studies have implicated a number of genes including ORMDL3, OPN3, PDE4D, TIM-1, GPRA, PHF11, DPP10 and ADAM33 which are associated with allergic asthma and asthmatic complications [73].
Obesity: Obesity can be defined as abnormal or excessive fat accumulation that may damage health. Percentage of body fat and BMI in Asian people is reported higher than in European populations [74].One fourth of Pakistani population is reported to be obese [75]. Although, there is not enough information regarding the genetic basis for the observed association between obesity and asthma yet obesity is considered as a major risk factor for asthma development. Severity of asthma in obese individuals is reported higher than in non-obese people and its response towards treatment is also very poor which makes it a major public health issue in many countries [76]. A study on 1,001 monozygotic and 383 dizygotic same-sex twin pairs reported that 8% of the genetic component of obesity was shared with asthma. It explained that the two diseases are associated strongly [77].
ASTHMA GENETICS STUDIES IN PAKISTAN
As already discussed asthma is a multi-factorial, polygenic complex disease and more than 100 genes have been reported as associated with asthma [78]. Asthma genetics of Pakistani population have been the ignored area in the studies. Recently some studies on asthma genetics have been completed in Pakistan reporting genetic association of SNP markers of genes CD-14 [79], IL-4 [80], IL-13 [81], ADAM33 [13] and locus 17q21 [9,82]. These studies were conducted on very limited scope and these don’t give much information regarding the genetics involved in this disease. Therefore there is a great potential and necessity to explore the genetics of asthma in Pakistani population. This may help to have a detailed data which might be helpful for better medical diagnostics and treatment of the disease afterwards.
ASTHMA MANAGEMENT GUIDELINES IN PAKISTAN
In Pakistan during 1983 chest physicians of the country gathered and decided to establish Pakistan Chest Society (PCS) without any government motivation. The objectives of this society were to conduct conferences and educational symposia for doctors and run various campaigns for patients and public health awareness regarding pulmonary diseases including asthma [83]. PCS published its own asthma guidelines in 2001 to steer the diagnosis and management of asthma in Pakistan. After it they didn’t further update or modify their document but latterly adopted GINA guidelines [84].
In 2013, Global Asthma Network carried out a short survey in 96 countries including Pakistan to know what types of guidelines are being followed worldwide. The results showed that 40% of countries developed their own guidelines for adult, children or both with or without assistance of pharmaceutical companies and exclusively used it [3]. It included some low and middle income countries like Ethiopia, India, Nigeria and Palestine. While the countries like Pakistan which have not developed their own guidelines, mostly implement Global Initiative for Asthma (GINA) guidelines and remaining use various others included British Thoracic Society (BTS), National Asthma Education and Prevention Program (NAEPP) and World Health Organization (WHO) released guidelines [3].
ASTHMA MANAGEMENT PLAN
At present asthma cannot be cured completely and only be controlled and managed so that patient can live a normal routine life by taking some precautions and awareness about the disease. All international guidelines categorized Diagnosis and Asthma management plan into four components.
i. Diagnosis: Diagnosing a patient as having asthma is only the first step in reducing the symptoms, functional restrictions, impairment in quality of life, and risk of adverse events of exacerbation. There is no single reliable test and there are no standardized diagnostic criteria for asthma. Asthma can be detected in a person by evaluating patterns of symptoms, physical examination and family history [85][113]. Spirometry is taken as the gold standard for the diagnosis of asthma, spirometer measures the speed by which lungs can be filled and emptied of air, giving an indication of how well lungs are performing or how much the bronchial tubes have narrowed. This enables a doctor to make decisions about lung condition and to plan the best treatment for patient. To confirm diagnosed asthma, the reversibility measures test of obstructive pulmonary tract is performed for which FEV1 (forced expired volume in one second) is measured before and 10 to 15 minutes after administering a metered dose of bronchodilator (Beta2 agonists e.g. salbutamol, terbutaline, etc.). A normal person shows smaller difference in both values (up to 8% in most studies) and in asthma patient FEV1 increase at least ≥200 mL and ≥12% from baseline after administration of bronchodilator [86-91].
Beside these typical tests sometimes others supplementary tests are performed which help to assess the severity of disease such as bronco provocation test to confirm bronchial hyper-responsiveness, allergy test to assess atopic asthma. Exhaled nitric oxide test is performed to suspect eosinophilic asthma, pulse oximetry and arterial blood gas analysis are used to evaluate the severity of acute asthma attack. Besides it, sometime chest X-rays are performed to rule out any other ailment with similar symptoms such as pneumothorax [4,90].
ii. Asthma self-management education plan: After the diagnosis of asthma in a person, physician develops an asthma management action plan to help the patient in administration of medicine and monitor the condition. Asthma self-management education plan is important for patients to learn skills necessary to good compliance of asthma therapy and improve outcomes [85,86].
iii. Environmental measures: Knowing the medical history of patient and his family those indoor and outdoor environmental allergens and conditions should be avoided that can induce or exacerbate asthma. Some factors are being advised to avoid completely such as first hand or second hand cigarette smoke, maintaining the dust mites, cockroaches, mold and pets free house environment, irradiate the exposure to pollens, household aerosols, perfumes, scents, fire smoke, outdoor industrial/traffic pollution, certain foods and medicines e.g. bee products, aspirin and cold drinks if patient is intolerant to them. Some suggestions are advised to specifically manage for an asthma patient. These advices may be to control and manage physical exercise, arousal of extreme emotions such as anger or fear, laughing and excitement, comorbid, some medical and physiological conditions such as allergic rhinitis, gastro-esophageal reflux disease, nasal polyposis, obesity and upper airway dysfunction pregnancy and sexual activity.
iv. Pharmacologic therapy: Asthma medicines are divided into two classes on basis of their pharmaco-action and severity and onset of symptoms. To control and manage chronic asthma long term drugs or preventers that minimize lung inflammation like inhaled corticosteroids (e.g. beclomethasone dipropionate, ciclesonide, fluticasone propionate, etc.), long-acting beta2 agonist (eformoterol fumarate dehydrate, Salmeterol xinafoate, etc.), leukotriene receptor antagonists (montelukast) and mast cell stabilizer cromones (Sodium cromoglycate, nedocromil sodium, etc.) are used. While in the treatment of acute symptoms and exacerbations quick-relief medications are used that induce the dilation of constraint airways and improve breathing called short term drugs or reliever such as short-acting beta2 agonist (salbutamol, terbutaline sulfate), inhaled corticosteroids (budesonide), anticholinergic bronchodilators (Ipratropium bromide) and magnesium sulfate containing drugs are suggested [83].
CURRENT SITUATION OF ASTHMA MANAGEMENT IN PAKISTAN
In previous two decades the understanding of epidemiology and management of asthma has increased reasonably but besides it, the asthma prevalence has been raised worldwide including Pakistan. This rise is ranging from 5% to almost 20% of the pediatric population in Pakistan [92]. The reported data is depicting asthma prevalence touching the alarming limits in all parts of Pakistan and casting fatal impacts on public health and the economy of the country [25].
Although asthma cannot be cured completely but appropriate management can control its severity and enable patient to enjoy good quality life [93]. Low literacy rate and lack of medical facilities due to negligible funding in the health sector by the governments has deteriorated the health situation in Pakistan. A few studies have been conducted in the last decade after publishing the international consensus guidelines to evaluate the management practices and medications prescribed by General Physicians and understanding level of patient’s family at very limited samples size by some students of teaching hospitals [92-94]. Recently some data have been published on genomic associations of asthma but again, because of targeting very small sample size and few genes or loci only [9], it does not depict the complete picture of the impact of genomic variations on asthma in Pakistani population.
Asthma management is difficult in children as compared to adults, while it is reported as most common chronic disease in children. Therefore despite the presence of international guidelines for management, the family physicians who are mostly accessed for treatment, encounter confusion about it both in acute exacerbations as well as in long term prevention [92]. Similarly the general practitioners in remote rural areas of the country do not apply recommended asthma management guidelines.
In Pakistan, asthma awareness in care takers, adult patients and parents of asthmatic children is inadequate as compared to the rest of the world [95]. There are several misconceptions and myths related to asthma attacks and their treatment in the country. For example, people thought rice and oily foods aggravate asthma and asthma was spread by physical contacts and they actually didn’t understand the importance of identification and avoidance of triggers for management of asthma. Very few people thought that asthma could be hereditary and thought it a contiguous disease [84]. People hesitate to accept the diagnosis of asthma and consider it a social stigma. So following are some recommendations to control the increasing number of asthma patients in Pakistan
- Although International asthma management guidelines address almost all aspects of disease but it is felt that awareness campaigns and training programs for general practitioners and carers of asthmatic patients are needed, so that these can be used to reduce the morbidity and mortality in addition to improving the quality of life of asthmatic patients.
- An extensive educational media campaign is required for awareness of the masses.
- The burden of asthma can markedly be reduced using strategies that have been adapted to the local societal, economic and health care environments.
- Poor compliance of guidelines is one of the major problems in treatment of asthma and lack of knowledge and understanding about the disease is the major reason for poor compliance. So an extensive effort on government level is required to control the number of asthmatics in Pakistan.
- There is a need for the development of a common national strategy and action plan by the government to combat the rising dilemma.
- It is also the responsibility of asthma experts and healthcare professionals to collaborate with government public health authorities and international organizations to improve efficiency in management and care of asthmatic persons in the community.
Researchers should investigate the genetic and genomic factors involved in the manifestation of this disease and their relations and associations with the specific environmental factors. They also need to know the changes in the cells and tissues and molecular expressions. These researches and studies must be resulted into the new targeted treatments of asthma.
Conflict of Interest Statement
The authors declare that they have no competing interests.
Funding
No funding was involved in this study. Institutional literature and internet resources were used.
References![]()
- Holgate ST. Pathogenesis of asthma. Clinical and Experimental Allergy, (2008); 38(6): 872-897.
- Rabasseda X. A report from the 2011 annual meeting of the american academy of Allergy, Asthma and Immunology (March 18-22, 2011 – San Francisco, California, USA). Drugs Today (Barc), (2011); 47(4): 313-323.
- Szefler SJ, Chmiel JF, Fitzpatrick AM, Giacoia G, Green TP, et al. Asthma across the ages: knowledge gaps in childhood asthma. Journal of Allergy and Clinical Immunology, (2014); 133(1): 3-13.
- Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma P. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy, (2004); 59(5): 469-478.
- Khawaja A, Shahzad H, Kazmi M, Zubairi AB. Clinical course and outcome of acute severe asthma (status asthmaticus) in adults. Journal of Pakistan Medical Association, (2014); 64(11): 1292-1296.
- Selgrade MK, Lemanske RF Jr, Gilmour MI, Neas LM, Ward MD, et al. Induction of asthma and the environment: what we know and need to know. Environmental Health Perspectives, (2006); 114(4): 615-619.
- Lee PY, Khoo EM. How well were asthmatic patients educated about their asthma? A study at the emergency department. Asia Pacific Journal of Public Health, (2004); 16(1): 45-49.
- Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulmonary Medicine, (2012); 12(1): 80.
- Shahid M, Sabar MF, Bano I, Rahman Z, Iqbal Z, et al. Sequence variants on 17q21 are associated with the susceptibility of asthma in the population of Lahore, Pakistan J Asthma, (2015); 52(8): 777-784.
- Asher MI. Urbanisation, asthma and allergies. Thorax, (2011); 66(12): 1025-1026.
- Weinberg EG. Urbanization and childhood asthma: an African perspective. Journal of Allergy and Clinical Immunology, (2000); 105(2): 224-231.
- Ghani MU, Sabar MF, Shahid M, Awan FI, Akram M. A report on asthma genetics studies in Pakistani population. Advancements in Life Sciences, (2017); 4(2): 33-38.
- Sabar MF, Ghani MU, Shahid M, Sumrin A, Ali A, et al. Genetic variants of ADAM33 are associated with asthma susceptibility in the Punjabi population of Pakistan. Journal of Asthma, (2016); 53(4): 341-348.
- Braman SS. The global burden of asthma. Chest, (2006); 130(1 Suppl): 4S-12S.
- Beasley R. The burden of asthma with specific reference to the United States. J Allergy Clin Immunol, (2002); 109(5 Suppl): S482-489.
- Mitchell EA. International trends in hospital admission rates for asthma. Arch Dis Child, (1985); 60(4): 376-378.
- Waqar MA, Khan M, Hasnain SM, Saleem A, Shaukat S, et al. Prevalence of Allergy and Asthma in School Children of Islamabad, Pakistan. World Applied Sciences Journal, (2009); 6(3): 426-432.
- Khan IA, Arsalan MH, Siddiqui MF, Zeeshan S, Shaukat SS. Spatial Association of Asthma and Vegetation In Karachi: A Gis Perspective. Pak J Bot, (2010); 42(5): 3547-3554.
- Hasnain SM, Khan M, Saleem A, Waqar MA. Prevalence of asthma and allergic rhinitis among school children of Karachi, Pakistan, 2007. J Asthma, (2009); 46(1): 86-90.
- Janahi IA, Bener A, Bush A. Prevalence of asthma among Qatari schoolchildren: International Study of Asthma and Allergies in Childhood, Qatar. Pediatr Pulmonol, (2006); 41(1): 80-86.
- Foliaki S, Annesi-Maesano I, Daniel R, Fakakovikaetau T, Magatongia M, et al. Prevalence of symptoms of childhood asthma, allergic rhinoconjunctivitis and eczema in the Pacific: the International Study of Asthma and Allergies in Childhood (ISAAC). Allergy, (2007); 62(3): 259-264.
- Ait-Khaled N, Odhiambo J, Pearce N, Adjoh KS, Maesano IA, et al. Prevalence of symptoms of asthma, rhinitis and eczema in 13- to 14-year-old children in Africa: the International Study of Asthma and Allergies in Childhood Phase III. Allergy, (2007); 62(3): 247-258.
- Kaur B, Anderson HR, Austin J, Burr M, Harkins LS, et al. Prevalence of asthma symptoms, diagnosis, and treatment in 12-14 year old children across Great Britain (international study of asthma and allergies in childhood, ISAAC UK). BMJ, (1998); 316(7125): 118-124.
- Leung R, Wong G, Lau J, Ho A, Chan JK, et al. Prevalence of asthma and allergy in Hong Kong schoolchildren: an ISAAC study. Eur Respir J, (1997); 10(2): 354-360.
- Ahmad F, Yousaf F, Asif S. Prevalence of Allergic Disease and Related Allergens in Pakistan in 2007. Journal of Postgraduate Medical Institute (Peshawar-Pakistan), (2011); 25(1).
- Asher MI, Weiland SK. The International Study of Asthma and Allergies in Childhood (ISAAC). ISAAC Steering Committee. Clin Exp Allergy, (1998); 28 Suppl 552-66; discussion 90-51.
- Khan U, Amir M, Khan M. Frequency of Asthma among students of Army Medical College. Ann Pak Inst Med Sci, (2011); 7(3): 142-145.
- Kumar A, Ghosh B. Genetics of asthma: a molecular biologist perspective. Clin Mol Allergy, (2009); 77.
- Louis R, Schleich F, Corhay JL, Louis E. Asthma: a complex disease determined by genetic and environmental factors. Rev Med Liege, (2012); 67(5-6): 286-291.
- Hirschhorn JN. Genomewide association studies–illuminating biologic pathways. New England Journal of Medicine, (2009); 360(17): 1699.
- Rosenwasser LJ. Genetics of asthma and atopy. Toxicol Lett, (1996); 86(2-3): 73-77.
- Harangi F, Lorinczy K, Lázár A, Orkényi M, Adonyi M, et al. Prevalence of childhood asthma in Baranya County, Hungary, between 2003 and 2006. Orvosi hetilap, (2007); 148(35): 1643-1648.
- Hassanzadeh J, Mohammadbeigi A, Mousavizadeh A, Akbari M. Asthma prevalence in Iranian guidance school children, a descriptive meta-analysis. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, (2012); 17(3): 293-297.
- Kumar GS, Roy G, Subitha L, Sahu SK. Prevalence of bronchial asthma and its associated factors among school children in urban Puducherry, India. Journal of natural science, biology, and medicine, (2014); 5(1): 59.
- Lima RG, Pastorino A, Casagrande R, Sole D, Leone C, et al. Prevalence of asthma, rhinitis and eczema in 6-7 years old students from the western districts of São Paulo City, using the standardized questionnaire of the" International Study of Asthma and Allergies in Childhood"(ISAAC)-phase IIIB. Clinics, (2007); 62(3): 225-234.
- Pakhale S, Wooldrage K, Manfreda J, Anthonisen N. Prevalence of Asthma Symptoms in 7 th-and 8 th-Grade School Children in a Rural Region in India. Journal of Asthma, (2008); 45(2): 117-122.
- Valdivia C, Caussade L, Navarro M, Cerda L, Pérez B, et al. Changes in asthma prevalence among school children during a 6-year period: Influence of socioeconomic status. Revista medica de Chile, (2009); 137(2): 215-225.
- Anderson H, Pottier A, Strachan D. Asthma from birth to age 23: incidence and relation to prior and concurrent atopic disease. Thorax, (1992); 47(7): 537-542.
- Nicolai T, Pereszlenyiova‐Bliznakova L, Illi S, Reinhardt D, Von Mutius E. Longitudinal follow‐up of the changing gender ratio in asthma from childhood to adulthood: role of delayed manifestation in girls. Pediatric allergy and immunology, (2003); 14(4): 280-283.
- Venn A, Lewis S, Cooper M, Hill J, Britton J. Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. Bmj, (1998); 316(7149): 1945-1946.
- Mustafa G, Khan PA, Iqbal I. Nocturnal asthma in school children of south Punjab Pakistan. J Ayub Med Coll Abbottabad, (2008); 20(3): 36-39.
- de Nijs SB, Venekamp LN, Bel EH. Adult-onset asthma: is it really different? European Respiratory Review, (2013); 22(127): 44-52.
- Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy, (2008); 63(1): 47-57.
- Vink NM, Postma DS, Schouten JP, Rosmalen JG, Boezen HM. Gender differences in asthma development and remission during transition through puberty: the TRacking Adolescents' Individual Lives Survey (TRAILS) study. Journal of Allergy and Clinical Immunology, (2010); 126(3): 498-504. e496.
- Dijk FN, de Jongste JC, Postma DS, Koppelman GH. Genetics of onset of asthma. Current opinion in allergy and clinical immunology, (2013); 13(2): 193-202.
- Moffatt MF, Gut IG, Demenais F, Strachan DP, Bouzigon E, et al. A large-scale, consortium-based genomewide association study of asthma. New England Journal of Medicine, (2010); 363(13): 1211-1221.
- Wan Y, Shrine N, Artigas MS, Wain L, Blakey J, et al. Genome-wide association study to identify genetic determinants of severe asthma. Thorax, (2012); thoraxjnl-2011-201262.
- Bisgaard H, Bønnelykke K, Sleiman PM, Brasholt M, Chawes B, et al. Chromosome 17q21 gene variants are associated with asthma and exacerbations but not atopy in early childhood. American journal of respiratory and critical care medicine, (2009); 179(3): 179-185.
- Ono JG, Worgall TS, Worgall S. 17q21 locus and ORMDL3: an increased risk for childhood asthma. Pediatric research, (2013); 75(1-2): 165-170.
- Naumova AK, Al Tuwaijri A, Morin A, Vaillancout VT, Madore A-M, et al. Sex-and age-dependent DNA methylation at the 17q12-q21 locus associated with childhood asthma. Human genetics, (2013); 132(7): 811-822.
- Sleiman PM, Flory J, Imielinski M, Bradfield JP, Annaiah K, et al. Variants of DENND1B associated with asthma in children. New England Journal of Medicine, (2010); 362(1): 36-44.
- Marat AL, McPherson PS. Variants of DENND1B associated with asthma in children. N Engl J Med, (2010); 363(10): 988-989.
- Schauberger EM, Ewart SL, Arshad SH, Huebner M, Karmaus W, et al. Identification of ATPAF1 as a novel candidate gene for asthma in children. Journal of Allergy and Clinical Immunology, (2011); 128(4): 753-760. e711.
- Mortensen LJ, Kreiner-Møller E, Hakonarson H, Bønnelykke K, Bisgaard H. The PCDH1 gene and asthma in early childhood. European Respiratory Journal, (2014); 43(3): 792-800.
- Li H, Li Y, Zhang M, Xu G, Feng X, et al. Associations of genetic variants in ADAM33 and TGF?? 1 genes with childhood asthma risk. Biomedical reports, (2014); 2(4): 533-538.
- Maalmi H, Beraies A, Charad R, Ammar J, Hamzaoui K, et al. IL-17A and IL-17F genes variants and susceptibility to childhood asthma in Tunisia. Journal of Asthma, (2014); 51(4): 348-354.
- Hirota T, Takahashi A, Kubo M, Tsunoda T, Tomita K, et al. Genome-wide association study identifies three new susceptibility loci for adult asthma in the Japanese population. Nature genetics, (2011); 43(9): 893-896.
- Yatagai Y, Sakamoto T, Yamada H, Masuko H, Kaneko Y, et al. Genomewide association study identifies HAS2 as a novel susceptibility gene for adult asthma in a Japanese population. Clinical & Experimental Allergy, (2014); 44(11): 1327-1334.
- Utsumi Y, Sasaki N, Nagashima H, Suzuki N, Nakamura Y, et al. Association of IL-13 gene polymorphisms with airway hyperresponsiveness in a Japanese adult asthmatic population. Respiratory investigation, (2013); 51(3): 147-152.
- Radhakrishnan AK, Raj VL, Tan L-K, Liam C-K. Single nucleotide polymorphism in the promoter of the human interleukin-13 gene is associated with asthma in Malaysian adults. BioMed research international, (2013); 2013.
- Zhu N, Gong Y, Chen X, Zhang J, Long F, et al. Association between the polymorphisms of interleukin-4, the interleukin-4 receptor gene and asthma. Chinese medical journal, (2012); 126(15): 2943-2951.
- Kuroshli Z, Gourabi H, Bazrgar M, Sanati MH, Bahraminejad E, et al. HLA-G allele and Haplotype Frequencies in a Healthy Population of Iran. Iranian Journal of Allergy, Asthma and Immunology, (2014); 13(3): 207.
- Piacentini S, Polimanti R, Iorio A, Cortesi M, Papa F, et al. GSTA1*‐69C/T and GSTO2* N142D as asthma‐and allergy‐related risk factors in Italian adult patients. Clinical and Experimental Pharmacology and Physiology, (2014); 41(3): 180-184.
- Taniguchi N, Konno S, Hattori T, Isada A, Shimizu K, et al. The CC16 A38G polymorphism is associated with asymptomatic airway hyper-responsiveness and development of late-onset asthma. Annals of Allergy, Asthma & Immunology, (2013); 111(5): 376-381. e371.
- Hizawa N, Makita H, Nasuhara Y, Hasegawa M, Nagai K, et al. Functional single nucleotide polymorphisms of the CCL5 gene and nonemphysematous phenotype in COPD patients. European Respiratory Journal, (2008); 32(2): 372-378.
- Spergel JM. From atopic dermatitis to asthma: the atopic march. Annals of Allergy, Asthma & Immunology, (2010); 105(2): 99-106.
- Rhodes HL, Sporik R, Thomas P, Holgate ST, Cogswell JJ. Early life risk factors for adult asthma: a birth cohort study of subjects at risk. Journal of allergy and clinical immunology, (2001); 108(5): 720-725.
- Rhodes HL, Thomas P, Sporik R, Holgate ST, Cogswell JJ. A birth cohort study of subjects at risk of atopy: twenty-two–year follow-up of wheeze and atopic status. American journal of respiratory and critical care medicine, (2002); 165(2): 176-180.
- Gustafsson D, Sjöberg O, Foucard T. Development of allergies and asthma in infants and young children with atopic dermatitis–a prospective follow‐up to 7 years of age. Allergy, (2000); 55(3): 240-245.
- Ohshima Y, Yamada A, Hiraoka M, Katamura K, Ito S, et al. Early sensitization to house dust mite is a major risk factor for subsequent development of bronchial asthma in Japanese infants with atopic dermatitis: results of a 4-year followup study. Annals of Allergy, Asthma & Immunology, (2002); 89(3): 265-270.
- Cookson WO, Moffatt MF. Genetics of asthma and allergic disease. Human molecular genetics, (2000); 9(16): 2359-2364.
- Illi S, von Mutius E, Lau S, Nickel R, Grüber C, et al. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. Journal of Allergy and Clinical Immunology, (2004); 113(5): 925-931.
- Agrawal DK, Shao Z. Pathogenesis of allergic airway inflammation. Current allergy and asthma reports, (2010); 10(1): 39-48.
- WHO EC. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England), (2004); 363(9403): 157.
- Jafar TH, Chaturvedi N, Pappas G. Prevalence of overweight and obesity and their association with hypertension and diabetes mellitus in an Indo-Asian population. Canadian Medical Association Journal, (2006); 175(9): 1071-1077.
- Dixon AE, Holguin F, Sood A, Salome CM, Pratley RE, et al. (2010) An official American Thoracic Society Workshop report: obesity and asthma. Proceedings of the American Thoracic Society. pp. 325-335.
- Hallstrand TS, Fischer ME, Wurfel MM, Afari N, Buchwald D, et al. Genetic pleiotropy between asthma and obesity in a community-based sample of twins. Journal of Allergy and Clinical Immunology, (2005); 116(6): 1235-1241.
- March ME, Sleiman PM, Hakonarson H. The genetics of asthma and allergic disorders. Discovery medicine, (2011); 11(56): 35-45.
- Micheal S, Minhas K, Ishaque M, Ahmed F, Ahmed A. Promoter polymorphisms of the CD14 gene are associated with atopy in Pakistani adults. (2011).
- Micheal S, Minhas K, Ishaque M, Ahmed F, Ahmed A. IL-4 gene polymorphisms and their association with atopic asthma and allergic rhinitis in Pakistani patients. J Investig Allergol Clin Immunol, (2013); 23(2): 107-111.
- Shazia M, Kanza M, Mehwish I, Irum S, Farida A, et al. IL-13 gene polymorphisms and their association with atopic asthma and rhinitis in Pakistani patients. Iranian Journal of Allergy, Asthma and Immunology, (2013); 12(4): 391.
- Sabar MF, Shahid M, Bano I, Ghani MU, Akram M, et al. rs12603332 is associated with male asthma patients specifically in urban areas of Lahore, Pakistan. J Asthma, (2017); 54(9): 887-892.
- PAKISTAN CHEST SOCIETY. http://www.pakistanchestsociety.pk/
- Zaman M, Ashraf S, Javaid M. Reliability of diagnosis and asthma knowledge, attitudes and perception (KAP) in rural population of NWFP, Pakistan. Pakistan Journal of Chest Medicine, (2015); 12(4).
- Education NA, Asthma PPTEPotMo Guidelines for the Diagnosis and Management of Asthma: Summary Report 2007. Chapter: Book Name. 2008 of publication; US Department of Health and Human Services, National Institues of Health, National Heart, Lung, and Blood Institute.
- Costain D, Harrison B, Holgate S, Hopkins A, Pattridge M. Guidelines for management of asthma in adults: I–Chronic persistent asthma. BMJ, (1990); 301(6753): 651-653.
- Guidelines for management of asthma in adults: II–Acute severe asthma. Statement by the British Thoracic Society, Research Unit of the Royal College of Physicians of London, King's Fund Centre, National Asthma Campaign. BMJ, (1990); 301(6755): 797-800.
- Scottish IGN. British guideline on the management of asthma. Thorax, (2003); 58i1.
- Network BTSSIG. British guideline on the management of asthma. Thorax, (2014); 69(Suppl 1): i1-i192.
- Bateman E, Hurd S, Barnes P, Bousquet J, Drazen J, et al. Global strategy for asthma management and prevention: GINA executive summary. European Respiratory Journal, (2008); 31(1): 143-178.
- Higgins B, Douglas J. The new BTS/SIGN asthma guidelines: where evidence leads the way. Thorax, (2003); 58(2): 98-99.
- Ahmed S, Ali R, Qadir M, Humayun K. Asthma in children: management issues for family doctors. Oman Med J, (2010); 25(4): 253-255.
- Organization WH. Global Alliance against Chronic Respiratory Diseases (GARD): general meeting report: Istanbul, Turkey, 30-31 May 2008. (2008).
- Hussain S, Zahid S, Khan J, Haqqee R. Asthma management by general practitioners in Pakistan. The International Journal of Tuberculosis and Lung Disease, (2004); 8(4): 414-417.
- Hazir T, Das C, Piracha F, Waheed B, Azam M. Carers’ perception of childhood asthma and its management in a selected Pakistani community. Archives of disease in childhood, (2002); 87(4): 287-290.
This work is licensed under a Creative Commons Attribution-Non Commercial 4.0 International License. To read the copy of this license please visit: https://creativecommons.org/licenses/by-nc/4.0